The diabetic patient with good oral health*
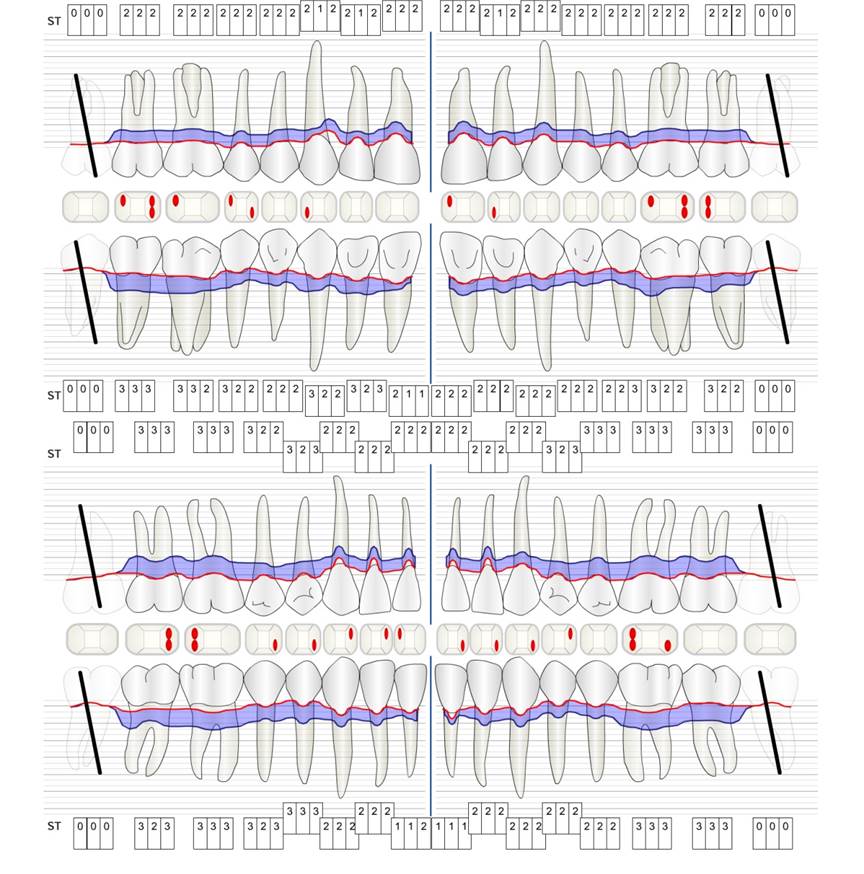
A 51-year old diabetic patient presents with good oral health at a prevention session. Her blood sugar levels are stable at HbA1c = 6.2%, and thus her condition is thought to be sufficiently managed with the antidiabetic drug metformin. The patient has no existing restorations or early oral disease. Using the dental results, it is possible to determine gingivitis in spite of an otherwise stable condition.

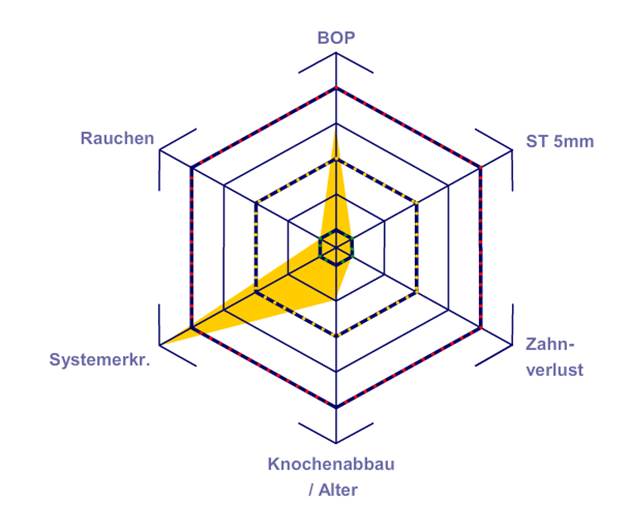
Despite the oral and general health parameters being stable, the patient’s underlying health condition requires her to attend a personalized prevention session. Diabetes mellitus is always associated with an increased risk of periodontitis (12). However, this can be controlled with good medicinal treatment. Regular monitoring of the HbA1c provides information about the course of the blood sugar level over the last eight to twelve weeks, with an HbA1c ≥ 6.5% indicating the presence of diabetes mellitus.

Because diabetes is so closely associated with periodontitis and has a significant impact on its development and progression, careful documentation is essential. Due to its significance, as described above, the patient should be asked for their current HbA1c value at every session.

The links between diabetes mellitus and the risk of periodontitis can be clearly explained during the consultation (12, 15), as can the impacts of a permanently elevated blood sugar level (hyperglycaemia) on the course and progression of periodontitis (16).

Even if the patient’s oral health gives no indication of any particular need for a shorter recall interval, twice-yearly prophylactic sessions are recommended due to the risks that come with diabetes mellitus and its association with an increased risk of periodontitis.
Individual Prophy Cycle – The patient-oriented prevention concept

Priv-Doz Dr Gerhard Schmalz is a senior physician at the Oral Health Medicine, Polyclinic for Dental Preservation and Periodontology, University Hospital Leipzig, Leipzig (Director: Prof Dr Rainer Haak).

Prof Dr Dirk Ziebolz MSc is a senior physician at the Polyclinic for Dental Preservation and Periodontology, Leipzig University Medical Centre (Director: Prof Dr R. Haak); with focus on interdisciplinary dental preservation and health services research.
List of references
- Chapple IL, Bouchard P, Cagetti MG, Campus G, Carra MC, Cocco F, et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. 2017;44 Suppl 18:S39-s51
- Schmalz G, Ziebolz D, Individualisierte Prävention-ein patientenorientiertes Präventionskonzept für die zahnärztliche Praxis, ZWR- Das deutsche Zahnärzteblatt 2020;129;147-156
- Fresmann S., So sieht eine durchdachtes Prophylaxekonzept aus; Dental Magazin: Deutscher Ärzteverlag GmbH; 2015
- Schmalz G, Ziebolz D, Individualisierte Prävention-fallorientierte Bedarfsprävention, ZWR- Das deutsche Zahnärzteblatt 2020;129;33-41
- Schmalz G, Ziebolz D, Individualisierte Prävention-Implikation allgemeingesundheitlicher Faktoren, ZWR- Das deutsche Zahnärzteblatt 2019;128;295-304
- Wang C, Zhao Y, Zheng S, Xue J, Zhou J, Tang Y, et al. Effect of enamel morphology on nanoscale adhesion forces of streptococcal bacteria: An AFM study. Scanning. 2015;37(5):313-21
- Pence SD, Chambers DA, van Tets IG, Wolf RC, Pfeiffer DC. Repetitive coronal polishing yields minimal enamel loss. Journal of dental hygiene: JDH. 2011;85(4):348-57.
- Kumar PS. From focal sepsis to periodontal medicine: a century of exploring the role of the oral microbiome in systemic disease. The Journal of Physiology. 2017;595(2):465-76
- Lalla E, Papapanou PN. Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nature Reviews Endocrinology. 2011;7:738
- Miller WR, Moyers TB. Eight Stages in Learning Motivational Interviewing. Journal of Teaching in the Addictions. 2006;5(1):3-17
- Paradigmenwechsel im Biofilmmanagement [Internet]. Spitta GmbH. 2014. https://www.pnc-aktuell.de/prophylaxe/story/paradigmenwechsel-im-biofilmmanagement__3512.html
- Christensen RP, Bangerter VW. Determination of rpm, time, and load used in oral prophylaxis polishing in vivo. J Dent Res. 1984; 63(12):1376-1382
- Graumann SJ, Sensat ML, Stoltenberg JL. Air polishing: a review of current literature. Journal of dental hygiene : JDH. 2013;87(4):173-80
- Bordoloi P, Ramesh A, Thomas B, Bhandary R. Epidemiological survey of dentinal hypersensitivity after oral prophylaxis. J Cont Med A Dent. 2018;6(1)
- James P, Worthington HV, Parnell C, Harding M, Lamont T, Cheung A, et al. Chlorhexidine mouthrinse as an adjunctive treatment for gingival health. The Cochrane database of systematic reviews. 2017;3:Cd008676
- Sawai MA, Bhardwaj A, Jafri Z, Sultan N, Daing A. Tooth polishing: The current status. Journal of Indian Society of Periodontology. 2015;19(4):375-80
- Slayton RL, Urquhart O, Araujo MWB, Fontana M, Guzman-Armstrong S, Nascimento MM, et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions: A report from the American Dental Association. J Am Dent Assoc. 2018;149(10):837-49 e19
- Gleissner E. Erfolgreiche Prävention auch in schwierigen Fällen. Allgemeine Zahnheilkunde: ZMK-aktuell; 2019
- Derks J, Schaller D, Hakansson J, Wennstrom JL, Tomasi C, Berglundh T. Effectiveness of Implant Therapy Analyzed in a Swedish Population: Prevalence of Peri-implantitis. Journal of dental research 2016;95:43-49
- Newton JT, Asimakopoulou K. Managing oral hygiene as a risk factor for periodontal disease: a systematic review of psychological approaches to behaviour change for improved plaque control in periodontal management. Journal of Clinical Periodontology 2015;42:S36-S46
- Veitz-Keenan A, James R, Implant outcomes poorer in patients with history of periodontal disease, Evicénce-Based-Dentistry 18, 5 (2017)



comments